One Doctor-Congressman Takes Aim at Prior Authorization
May 7, 2025 | by ltcinsuranceshopper

Rep. Mark Green, a Tennessee Republican, made a dramatic late-life decision to become a physician while he was serving as a captain in the U.S. Army’s storied 82nd Airborne Division. After surgeons saved his father’s life in an emergency, Green asked the military to send him to medical school, and they agreed.
On his new path, Green served as a special-operations flight surgeon in the wars in Iraq and Afghanistan, then founder and CEO of an emergency-room staffing company. He was eventually propelled into politics – winning election to the U.S. House in 2018.
Now, as a leader of the GOP Doctors Caucus in the House, Green has put his political clout behind a bill targeting a crucial concern of doctors and patients: Insurance companies’ prior approval practices that too often delay or deny coverage for essential medications or procedures.
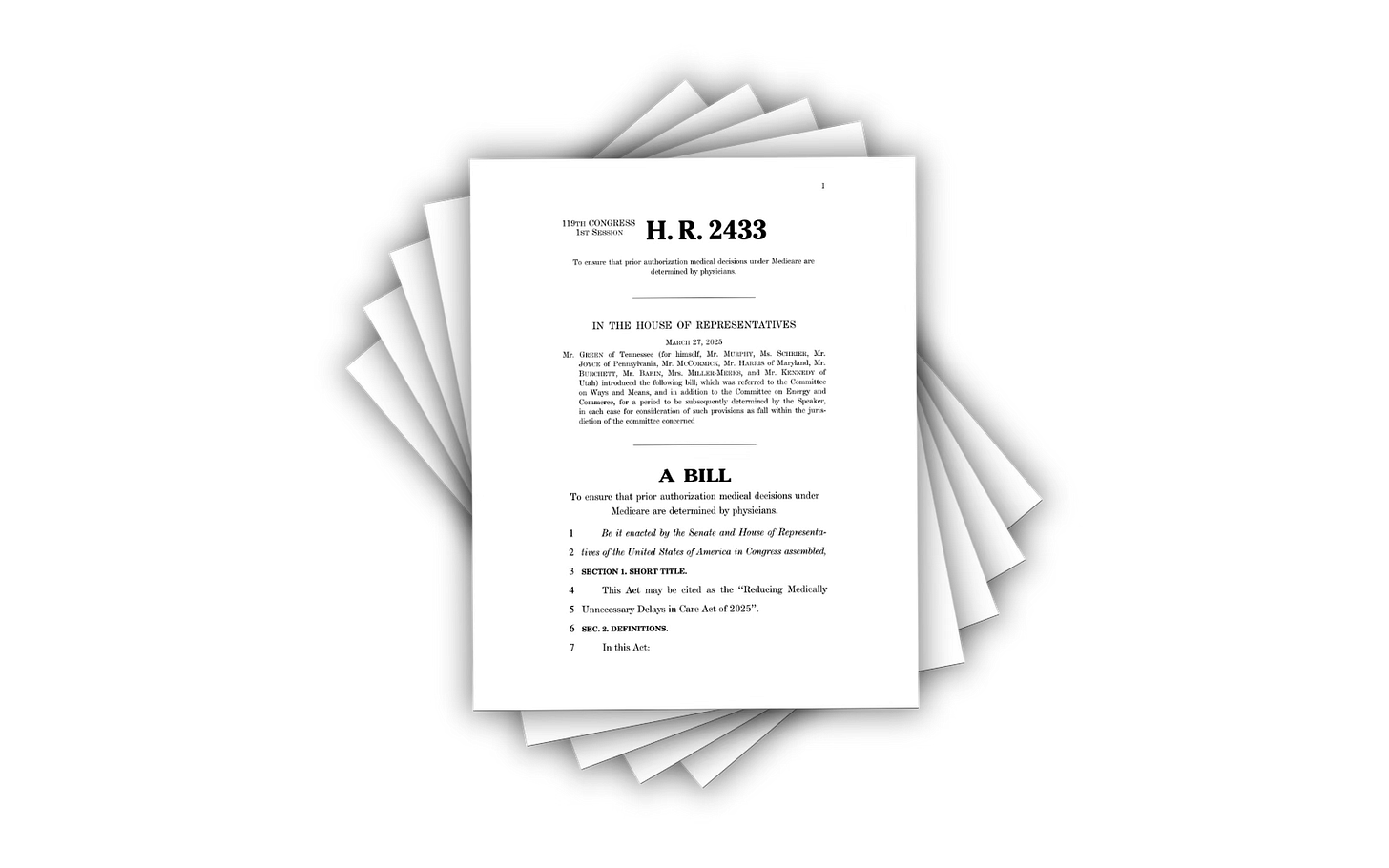
The Green-sponsored Reducing Medically Unnecessary Delays in Care Act of 2025 aims to streamline the process by requiring that board-certified physicians in the same specialty as a patient’s claim are making the decisions for insurers – not always the case now. It also aims to reform the use of prior authorization throughout the vast Medicare system so that decisions are made only on the basis of medical need and best practices.
“As a physician, I’ve seen first-hand how prior authorization has affected patient care,” Green said in an email interview. “Additionally, as a cancer survivor myself, I know how important screenings like colonoscopies are. I don’t think ineffectual bureaucratic hoops should get in the way of saving lives.”
This isn’t the first time that either Green or his allies in Congress have attempted to take on the insurance lobby and address what many doctors and their patients agree is an increasing obstacle to getting the best, and most timely, medical care.
Recently, the national conversation about Big Insurance practices was refocused by a tragic event. December’s assassination of UnitedHealthcare CEO Brian Thompson by alleged gunman Luigi Mangione prompted an outpouring of horror stories from Americans about their dealings with large insurance companies – many of them around prior authorization hassles. (The shell casings and a bullet from the gun used in the shooting had the words “deny,” “defend” and “depose” written on them, similar to terms used by critics to accuse insurers of delaying or denying claim payments.)
Currently, it’s estimated that the private health insurers who cover some 200 million Americans reject as many as one of every seven claims submitted to them – often insisting the proposed treatment is experimental or isn’t covered for the relevant illness. Yet one recent report found that a miniscule 0.1 percent of prior-authorization rejections are ever challenged by patients.
And there is mounting evidence that big insurers aren’t asking doctors with the right expertise to review the cases they reject, or even that much time is spent on the claims at all. ProPublica’s investigation into claim-denial practices cited one Cigna medical director who personally rejected 60,000 claims in one month, and who typically did not even read them.
The prior authorization bill co-sponsored by Green – with support from a Democratic physician in Congress, Rep. Kim Schrier of Washington state, as well as Rep. Greg Murphy of North Carolina, co-chair of the GOP Doctors Conference – targets that issue, and Green is hopeful that attacking health care inefficiencies and delays will attract more bipartisan support.
“This isn’t a new issue for me, but it’s one I am fully committed to — no matter how long it takes,” Green said. “I ran a medical staffing company after my military service and before running for Congress. When I see a need or an inefficiency, it’s in my nature to fix it — and that’s what I’m trying to do with prior authorization. I want to make our medical system as good as it can possibly be, one reform at a time.”
One survey by the American Medical Association (AMA) found that physicians and their staffs reported an average of 13 hours a week per doctor spent completing prior authorization paperwork, while 89% of doctors said prior authorization tasks somewhat or significantly increase physician burnout.
In addition to the AMA, the Green-backed prior authorization bill is backed by a broad medical coalition that includes the American Osteopathic Association, American College of Emergency Physicians, American College of Physicians, and the American Academy of Family Physicians, as well as several dozen groups representing doctors from many of the leading specialties.
“The American College of Physicians strongly opposes prior authorization requirements that are overly burdensome and pull physician time away from where it should be, on caring for our patients,” the president of the ACP, Dr. Isaac O. Opole, wrote. “These bureaucratic delays in care are especially galling when decisions about needed care are not being reviewed by physicians who are trained and knowledgeable in that care.”
But even widely popular health care reforms have struggled to get out of a deeply divided Congress in recent years. In January, legislation to reform practices by pharmacy benefit managers, or PBMs, gained significant bipartisan support but disappeared in the final days of that session after Elon Musk, who’s in charge of President Trump’s Department of Government Efficiency, led an intervention.
In the new session, advocates are optimistic but cautious. Peggy Tighe is a veteran Capitol Hill lobbyist who speaks for the Regulatory Relief Coalition, a partnership of medical specialties that endorsed the Green legislation shortly after it was introduced, even as it continues to also push for more aggressive prior authorization reforms.
The current state of prior authorization, Tighe said in an interview, “really drives doctors nuts. For example, if you’re an oncologist and you’re calling the insurance company saying I need a PET scan because this tumor is growing – I can tell it’s growing, I can feel it, but I need a PET scan to see what’s going on, and this person needs it right away. And the insurer says, ‘OK, well, it’s going to be delayed six weeks.’” Often, she added, doctors learn the case wasn’t even reviewed by someone in the relevant specialty.
“It’s no secret that health care has remained a contentious issue between Republicans and Democrats, but at the end of the day, my bill is about saving lives,” Green said. “No one wants to hear from an insurance company that their treatment isn’t covered by insurance. We can all relate to this — on both sides of the aisle.”
Tighe said her coalition continues to support a separate piece of legislation known as the Seniors’ Act, or Improving Seniors Timely Access to Care Act, that also targets the Medicare program with an aggressive overhaul of prior authorization practices.
Green believes public unrest over computer-driven decisions in health care may have reached a tipping point. “Pretty much everyone I speak with agrees that board-certified physicians in the same specialty should be the ones making the ultimate decisions about the best care for their patients,” he said. “The reality is that many insurance companies are completely detached from the human aspect of medicine. (Artificial intelligence) algorithms and number crunchers reading off a sheet of paper should not have the authority to supersede a trained physician.”
RELATED POSTS
View all