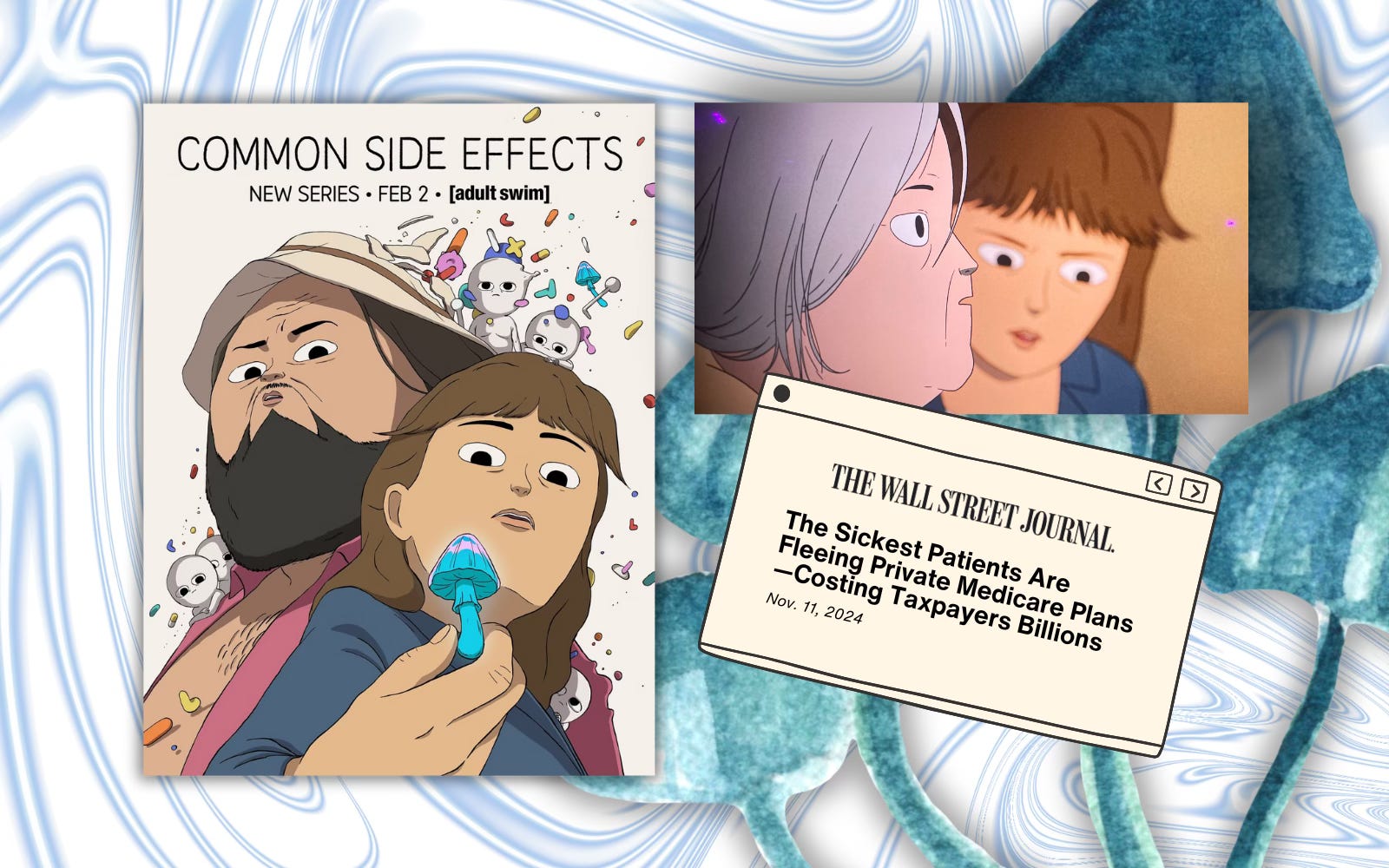
Adult Swim’s Common Side Effects Show Pitfalls of Medicare Advantage
February 12, 2025 | by ltcinsuranceshopper

I love cartoons. I considered Bugs Bunny a close, personal friend when I was a kid. I’ve watched Hotel Transylvania a dozen times with my grandkids. That’s why I started watching the new Adult Swim cartoon, Common Side Effects. The show follows once-separated high school friends Marshall, a mycologist, and Frances, the executive assistant to a pharmaceutical executive, who reconnect after Marshall begins peppering Frances’ boss with questions during a public event announcing a new drug the pharmaceutical company is launching.
I won’t get into the plot of the show (it involves Marshall’s discovery of a magic mushroom that seemingly can cure any alignment, and the chaos that follows his finding). As much as I’d like it to be, this post isn’t going to be about trippy truffles or freaky fungus – instead it’s about a quick scene wedged in the beginning of episode 3 involving Frances visiting her mother at what appears to be a skilled nursing facility.
Here’s a transcription of the scene between Frances and a nurse at the facility:
Nurse: Oh, Frances! Don’t usually see you during the week. Visiting hours are almost over, but –
Frances: Yeah, look. I know. I just… I just really want to see my mom.
Nurse: Okay. We do need to talk to you, though, about that, actually. Given your mom’s condition, they want to move her to a different facility, but –
Frances: What! No! No. We can’t move her. I… Look. I called about this. I spoke with the person – I think it was Diane – who runs…
Nurse: Okay, Frances. That’s the facility. But this is an insurance issue, and if they’re not gonna cover it, we need to know because –
Frances: God. Okay. Okay. Look. I will get the money somehow. Okay?
While there is no mention of the type of insurance Frances’s mom has, it’s most likely a Medicare Advantage plan because traditional Medicare wouldn’t force her mom to move. Medicare Advantage plans have limited and ever-changing networks of physicians, hospitals and other health care facilities.
That means that people enrolled in those plans, which are operated by private insurance companies, often have to change doctors and stop going to some hospitals or face steep out-of-pocket expenses. Traditional Medicare, on the other hand, doesn’t even have “networks”. Almost all health care providers in the United States accept traditional Medicare, which never forces patients to change from one provider to another.
Unfortunately, many seniors and their families are duped by slick Medicare Advantage ads for big insurance companies like UnitedHealthcare and Humana (where I used to work) that promise some additional benefits but that leave out important details, like often skimpy provider networks that change from year to year.
And no one’s immune from the Medicare Advantage duping. Not even me.
My mom was one of millions of seniors lured into a Medicare Advantage plan. It was fine until she broke her hip and needed skilled nursing care for rehab. Then she found out the best facilities were not in her insurer’s network. We had to get her out of that plan and get her enrolled in traditional Medicare so she could get the care she needed at a high-quality facility near her home in Tennessee.
What’s happening to Frances’ mother in Common Side Effects is exactly what my mom faced.
Know this: While it is possible to escape from a Medicare Advantage plan, it’s not as easy as you might think. A problem a lot of seniors in that predicament encounter is the challenge of finding an affordable Medicare supplement policy to cover out-of-pocket expenses. It gets complicated – and expensive – in a hurry.
RELATED POSTS
View all